Academic Medicine’s Triple Aim: Rethinking Compensation for Research, Teaching, and Care
Learn how AMCs can build fair, compliant compensation models that support their mission and financial stability.
Academic medicine is where healthcare’s brightest minds meet its biggest challenges. At the heart of this field are academic medical centers (AMCs)—hospitals affiliated with medical schools or universities, where physicians treat patients, conduct research, and train the next generation of doctors.
This triple mission sets AMCs apart from other hospitals but also creates a distinct challenge: how do you pay a clinician who spends half the week in the clinic, a quarter in the lab, and the rest teaching residents while sustaining success across the organization? Many physician compensation models remain anchored to clinical productivity metrics designed for simpler practice environments.
The solution is to treat compensation as a strategy. By grounding pay in valuation principles, AMCs can build fair, compliant compensation models that reward the full spectrum of faculty contributions, ensuring both financial sustainability and mission-driven impact.
The Unique Structure of Academic Medicine
Academic medicine operates under a three-part mission: patient care, research, and teaching. It’s what differentiates AMCs from community hospitals and private practices and what makes them indispensable to healthcare innovation.
Where community medical centers and private practices focus on routine care, AMCs take on a wider range of specialized care and treat more complex cases. They also serve as the training ground for future clinicians and the testing ground for tomorrow’s therapies.
That complexity comes at a cost. Research programs depend on external funding that rarely covers full program expenses. Faculty time spent supervising residents can reduce clinical productivity compared with non-academic centers. And higher patient care costs at AMCs may drive some patients to seek care elsewhere.
AMCs also see a higher proportion of Medicare and Medicaid patients, provide roughly 30% of all hospital-based charity care while representing only 5% of non-federal hospitals, and rely less on high-margin commercial payers. The result is a model that’s as mission-driven as it is margin-challenged, yet it’s what allows AMCs to advance medicine in ways that few other institutions can.
Funding Sources: What Fills the Bucket
AMCs draw from a mix of revenue sources to sustain their operations and compensate the faculty who make their mission possible. The main streams include:
- Clinical revenue: Income from patient services forming the backbone of AMC operations.
- Institutional support: University or hospital funds that underwrite teaching and research not fully covered by other sources.
- Grants: External dollars from government agencies, foundations, or industry to support research, usually covering only part of total costs.
- Graduate medical education (GME) funding: Federal payments for residency and fellowship programs.
- Endowments and philanthropy: Donor-driven resources for faculty positions, research, infrastructure, or strategic programs.
Understanding what funds are available is one challenge; understanding how they move through the organization is another. Funds flow describes how revenue circulates across departments, programs, and projects within an AMC. It tracks where money originates and how it’s allocated, but it does not directly determine what individual physicians earn.
Faculty compensation plans define how individual physicians are paid based on their specific work allocation. These plans translate a physician’s full-time equivalent (FTE) split across activities into actual compensation, drawing from the appropriate funding sources.
Challenges in Faculty Compensation
Balancing fair faculty pay against complex, unpredictable funding streams is an ongoing challenge for AMCs, as each revenue source has its own constraints.
Fluctuating clinical revenue. Clinical revenue is often the largest contributor to faculty pay, but it can fluctuate. Declining Medicare and Medicaid reimbursement, combined with commercial insurance delays and denials, makes it difficult to forecast or maintain consistent salary support tied to patient care.
Uncertain research funding. Research grants are competitive and time-limited, requiring investigators to continually secure new awards to maintain salary coverage. Funding lapses can force AMCs to bridge gaps to retain researchers, straining institutional reserves.
Limited institutional support. University and hospital funds that help underwrite non-clinical work are finite and often don’t keep pace with inflation. The result is growing pressure on AMCs to do more with less and to find ways to fund academic and leadership roles without overrelying on clinical dollars.
Talent retention under pressure. When teaching and grant-funded work are undervalued compared to clinical activities, faculty may gravitate toward revenue-generating roles or leave academic medicine. That imbalance threatens not only recruitment and retention, but also the long-term mission of education and discovery that defines the AMC model.
Together, these challenges underscore the need for compensation strategies that balance financial pragmatism with mission alignment, ensuring that faculty are rewarded not only for the care they deliver but for the scholarship and mentorship that sustain academic medicine.
Aligning Compensation with Faculty Work
Fair compensation plans start with a clear understanding of faculty work. The CARTS framework offers a standardized way to break down that effort and define FTE allocation across five components: Clinical, Administrative, Research, Teaching, and Strategic.
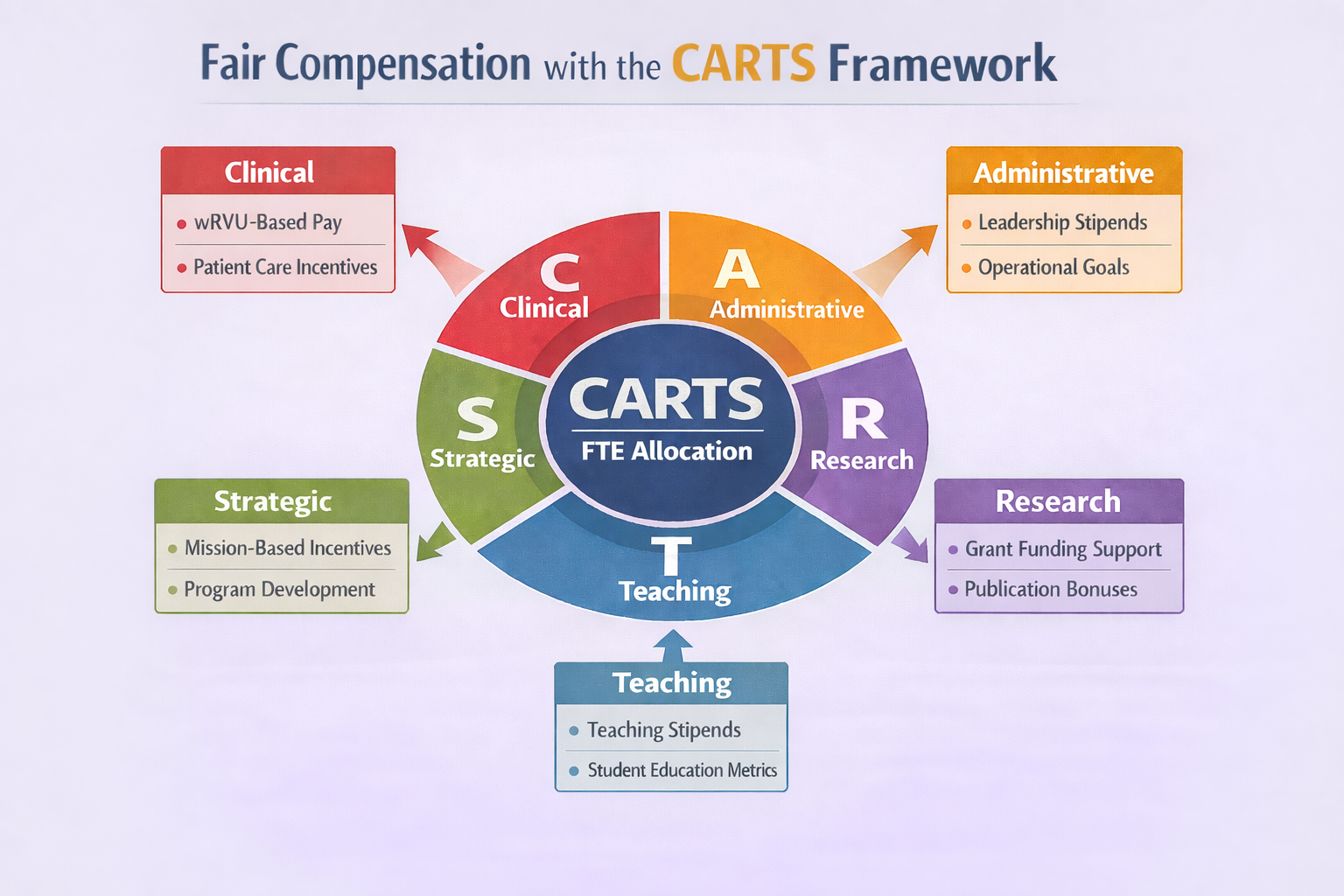
This framework serves two key purposes: it defines a physician’s FTE allocation and standardizes effort expectations across all activities, ensuring consistent evaluation, and it aligns compensation with actual work, preventing any component from being over- or undervalued.
Consider these examples:
- Physician A: 100% clinical FTE → Salary based on work relative value units (wRVUs) using industry-standard physician compensation benchmarks.
- Physician B: 50% clinical, 50% research → Compensation split between fair market value (FMV) clinical compensation and research funding.
When FTE allocations are vague or vary widely between departments or roles, several issues can arise. Overvaluing clinical output may trigger FMV violations, while undervaluing non-clinical work can cause faculty dissatisfaction and retention problems. Inconsistent FTE calculations can also create departmental inequities.
Defining FTE accurately ensures compensation models function properly and align with institutional priorities and revenue realities. A standardized CARTS model brings clarity to faculty expectations and fosters internal equity, while ensuring every dollar of compensation can be traced back to a defensible funding source.
Why Valuation Matters in Academic Medicine
Valuation is the backbone of fair, sustainable compensation. Done right, it balances three goals:
Legal & Compliance: Ensures pay arrangements meet Stark Law and Anti-Kickback Statute standards. For example, paying a faculty member above market rates for low clinical effort could trigger an indirect kickback risk, while overcompensating a high-referral physician above FMV could lead to Stark Law clawback violations. Clear valuation protects institutions and keeps compensation defensible.
Equity: Promotes consistency across departments and roles. By standardizing FTE allocations through tools like the CARTS framework, institutions can recognize all faculty work contributions. This prevents undervaluing non-clinical work and creates fairness across faculty roles and departments, reducing dissatisfaction.
Strategy: Aligns compensation with institutional goals and revenue realities. Effective valuation uses both non-academic benchmarks to answer “what can you pay?” and academic compensation data to answer “what should you pay?”
Valuation, in short, keeps the academic mission financially and ethically sound. And it sets the stage for the next question every AMC faces: not just what can we pay, but what should we pay.
What Can You Pay vs. What Should You Pay
Two questions drive compensation analysis in academic medicine, each with different implications.
“What can you pay?” FMV analysis provides a compliance-focused lens for establishing defensible payment ranges, drawing on benchmark data from sources like AMGA, MGMA, and SullivanCotter. This broader market view helps establish FMV parameters within market norms.
“What should you pay?” is strategic. Academic-specific compensation data, broken out by factors like faculty rank and organization size, offers nuanced insight into pay norms and productivity output, providing a talent- and mission-focused lens to guide competitive compensation strategies.
The strongest models balance both perspectives: Non-academic benchmarks ensure compliance and defensibility, while academic data guides more strategic decisions. Together, they create compensation structures aligned with the AMC’s broader mission.
Final Thoughts
Compensation in academic medicine isn’t just a cost center. It’s how AMCs advance their mission. Well-structured, valuation-driven models ensure faculty are rewarded fairly for their diverse contributions while maintaining compliance and fostering sustainability. AMCs that get this right don’t just retain top talent—they build enduring institutions that steer healthcare forward.
Explore how we help academic medical centers design fair, compliant compensation models.
